Big Pharma Drastically Overcharges the US Military
A government-granted monopoly has allowed a pharmacy benefit manager owned by Cigna to overbill the Defense Department for years, in what amounts to an enormous cash transfer from American taxpayers to Big Pharma’s shareholders.

It’s not breaking news that the US has a bloated military budget. But taxpayers may be interested to know that some of that money goes to pharmaceutical intermediaries who vastly overcharge the military for medicines. (Liu Jin / AFP via Getty Images)
One of the nation’s most powerful pharmacy intermediaries is quietly charging the military’s health insurance program $484 more on average per generic drug than independent and big chain pharmacies, according to exclusive data shared with The Lever. The scheme forces taxpayers to spend significantly more to inflate the company’s profits, while cutting off many military families from local, accessible pharmacy care.
Lawmakers are working to add language to the pending defense spending bill that could shed light on this overbilling by requiring the US Department of Defense to finally disclose how much it’s paying pharmacies for medicines. But standing in the way is the formidable lobbying arm of the pharmacy giant’s corporate owner, which has spent millions on military health insurance and other issues over the past six years.
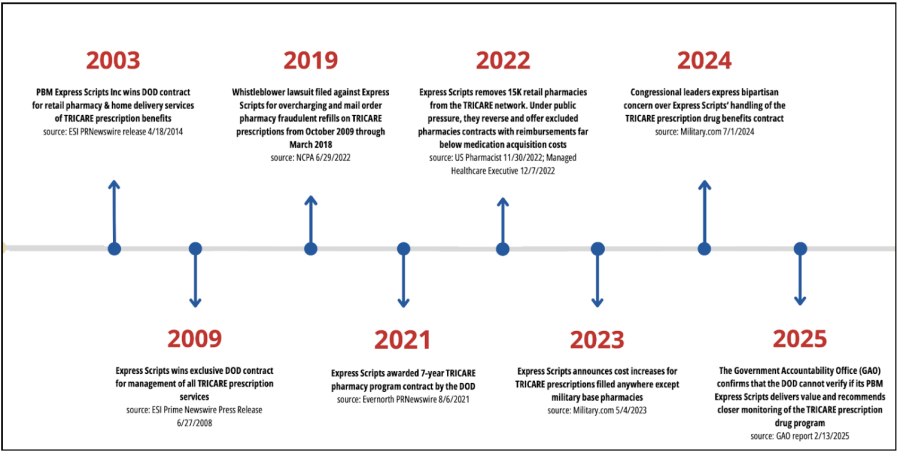
Express Scripts — a pharmacy benefit manager owned by health insurance giant Cigna — has overseen pharmacy benefits for the military’s health insurance program, TRICARE, since 2003. The program serves more than nine million active-duty service members, retirees, and their families.
This government-granted monopoly has allowed the company to “steer patients to its own pharmacy while disadvantaging competitors” and charge significantly more for commonly used generic drugs, according to a 2024 letter by lawmakers to the Department of Defense.
It’s difficult to know how much excess profit Express Scripts has netted from the arrangement. Despite years of bipartisan complaints and requests for more information by independent pharmacists, there’s been no effort to collect comprehensive data on the total amount Express Scripts is charging TRICARE for the drugs it provides up to this point.
“This is happening with a government-funded contract where things are supposed to be transparent,” said Monique Whitney, executive director of Pharmacists United for Truth and Transparency, an advocacy group that supports independent pharmacies. “Why are we seeing these prices?”
A spokesperson from Express Scripts said that this pricing analysis, which used drug costs listed on TRICARE’s online patient platform, is “inaccurate.”
“We have been made aware that it is displaying an inaccurate number for ‘what my plan pays’ for certain medicines dispensed to TRICARE beneficiaries,” an Express Scripts spokesperson wrote in an email to The Lever. “We are making updates to the tool.”
The company did not respond to follow-up questions requesting details about this inaccuracy.
Whitney questions Express Scripts’ claim. “Why would you put such widely inaccurate numbers up?” she said. “These are all questions that, if I were the Department of Defense, are the first things I would be looking at, because all evidence shows [Express Scripts] has been ripping the department off for forever.”
Years of Contracts
Pharmacy benefit managers act as middlemen between drug manufacturers and health insurers, determining which drugs the insurer will cover and how much they will cost. All of the top pharmacy benefit managers — Express Scripts, CVS Caremark, and OptumRx — are owned by major health care companies, giving these corporations control over almost every stage of the drug-pricing process.
In 2003, the Department of Defense awarded Express Scripts its first contract to manage the TRICARE pharmacy home delivery program. According to a February report by the US Government Accountability Office, a congressional watchdog, the move was made “with the goal of improving service for beneficiaries and saving money for military families and taxpayers by creating a more efficient, competitively priced pharmacy network.”
Nearly five years later, Express Scripts won another contract to manage all TRICARE prescription services, including specialty medications for complex medical conditions. Then, in 2021, they received a multiyear, $4.3 billion contract with the Department of Defense.
A year later, in October 2022, the company cut fifteen thousand pharmacies from the TRICARE network, many of which were small, independent drugstores. The move may have forced three hundred eighty thousand beneficiaries to find a new drugstore or switch to a mail-order pharmacy owned by Express Scripts, such as Accredo, according to a Government Accountability Office report.
The development triggered outcry among dozens of members of Congress from both parties. “What reasons has Express Scripts given [the Defense Health Agency] for terminating the 2022 [pharmacy] contracts early?” the lawmakers asked in a letter to the then acting assistant secretary for health affairs at the Defense Department. “This will only further reduce the pharmacy network for TRICARE patients and their families, and may force beneficiaries to change pharmacies at a time when many receive annual vaccinations.”
Thanks to public pressure, the pharmacy benefit manager eventually offered the pharmacies a chance to rejoin the TRICARE network — but it then instituted a broad increase in prescription drug co-pays.
Beyond the convenience of prescriptions delivered to their door, military families have another incentive to opt for Express Scripts’ mail-order services: The program allows them to receive a ninety-day supply of medications when filling a prescription, while other in-network pharmacies can only provide up to a thirty-day supply.
But those perks come with a price: By limiting pharmacy access and steering patients to in-house services, Express Scripts gets to pocket more money.
“Express Scripts can underreimburse the other pharmacies and give inflated payments to its corporate cousin, Accredo,” Senator Elizabeth Warren (D-Mass.) said during a Senate Special Committee On Aging hearing this October.
In an email to The Lever, an Express Scripts spokesperson stated that “Express Scripts does not direct beneficiaries to use a TRICARE Mail Order Pharmacy… outside of the government’s direction.”
For years, stakeholders have been calling on the Pentagon to disclose exactly how much Express Scripts has been earning thanks to its tightening grip on service members’ prescriptions.
“Right now, the Department of Defense refuses to check how much it is costing taxpayers in TRICARE,” said Warren during the Senate committee hearing earlier this month. “I’m pushing [the Department of Defense] to audit this information every single year.”
Inflated Costs
The lack of government action on exposing Express Script’s TRICARE profits inspired independent pharmacies to dig into the matter themselves.
This summer, the Pharmacists United for Truth and Transparency advocacy group launched a campaign to reveal the prices Express Scripts charges the federal government by analyzing pricing data provided through the online TRICARE patient portal. The group found that the company bills TRICARE significantly more for common generic drugs than other drugstores.
In Colorado, for example, the group found that Express Scripts’ mail-order pharmacy charges TRICARE $121.37 for a generic blood pressure medication, while major pharmacy chains, including CVS and Walgreens, charge anywhere from $3.47 to $4.96 for the same product.
In California, meanwhile, Express Scripts receives 162 times more from TRICARE than independent pharmacies for a generic antidepressant used by approximately 5.7 million patients nationwide. Such medication is particularly crucial for active duty members and veterans, who are more likely to suffer from depression and post-traumatic stress disorder than the general public.
The independent pharmacy group found similar price hikes in states nationwide, said Whitney, the organization’s executive director.
“This is how [pharmacy benefit managers] are structured so that they can get their money,” said Whitney. “They make a big effort to move beneficiaries to their own pharmacy and undercut other pharmacies in the network.”
Not only is the government paying Express Scripts more than other pharmacies, but military families are shelling out more money, too. Data from TRICARE’s website show that patients using its mail-order service often face higher co-pays for common drugs. For example, a generic cholesterol medication costs beneficiaries $13 through Express Scripts — compared to just $1.63 at Walgreens.
And these costs are set to rise: Yesterday, it was announced that TRICARE beneficiaries who fill their prescriptions outside of a military pharmacy will pay up to nearly 16 percent more in co-pays in 2026.
It’s well known that independent pharmacies have lower co-pays for many common drugs than Express Scripts’ mail-order options, said Mark Cuban, a businessman and television personality who runs the independent online pharmacy Cost Plus Drugs, during the Senate committee hearing. “It’s obvious that we’re cheaper.”
Mounting Pressure
In September, Representative Jen Kiggans (R-Va.) proposed an amendment to the House version of the latest defense spending bill to improve the TRICARE system for military families — but it was stripped before the bill passed.
“My proposal would have required fair and transparent reimbursement for local pharmacies, banned hidden fees that drive up costs, mandated independent audits of TRICARE’s pharmacy benefit managers, and protected patient choice so military families can keep using their trusted local pharmacies,” Kiggans wrote in an email to The Lever. “Although it wasn’t included in the House-passed [National Defense Authorization Act], I’ll keep fighting to make TRICARE more transparent, accountable, and supportive of the families who serve.”
Lawmakers are still working to add language to the final defense spending bill that would require TRICARE to reveal how much it’s paying different pharmacies. But any such efforts will likely encounter industry pushback.
Express Scripts’ parent company, Cigna, has lobbied on matters including “pharmacy issues related to TRICARE” and the National Defense Authorization Act consistently since 2019 — the same year a whistleblower lawsuit was filed against Express Scripts alleging the company over-delivered prescription drugs to TRICARE beneficiaries, defrauding the government and overcharging taxpayers by billions of dollars. Overall, the multibillion-dollar company has spent nearly $40 million on lobbying over the past six years, according to government records.
That level of influence raises concerns among advocates like Whitney.
“We want [military members] to have the best benefits available, but also for us as taxpayers, we want to know that our taxes are going to provide care and quality medications,” said Whitney. “We do not want our tax dollars going to pay shareholder dividends, which is so clearly happening here.”